Hip Surveillance in Cerebral Palsy
Hip Surveillance in Cerebral Palsy
- Section I: Evidence Summary
- Section II: Published Evidence
- Section III: Practical Tools
- Section IV: Acknowledgments
- Feedback/
Comments
Section I: Evidence Summary Printer Friendly Version
Definitions
Hip surveillance is defined as: “The process of monitoring and identifying the critical early indicators of hip displacement." Hip displacement refers to the displacement of the femoral head laterally out of the acetabulum and is measured using a migration percentage (MP). Hip subluxation refers to hip displacement where the femoral head is partially displaced from under the acetabulum while hip dislocation refers to hip displacement where the femoral head is completely displaced from under the acetabulum.
Impact: Why is Hip Surveillance Important
- Hip displacement and dislocation can lead to pain, reduced function and reduced quality of life.
- Children with cerebral palsy (CP) have an increased likelihood of hip displacement.
- Hip surveillance allows for early detection of hip displacement.
- Early detection enables referral for assessment and/or management.
- Hip surveillance for children with CP should be completed using a systematic approach.
Target Population: Pediatric/Children & Youth Population (age =19 years) diagnosed with CP or those children not yet diagnosed with CP but for whom there is a clinical suspicion of having CP.
Target Clinical Providers: Pediatricians including Pediatric Sub-Specialists, Radiologists and Pediatric Orthopedic Surgeons, Therapists, Radiology Technicians, and Nurses providing musculoskeletal care for children/youth with CP.
Assessment
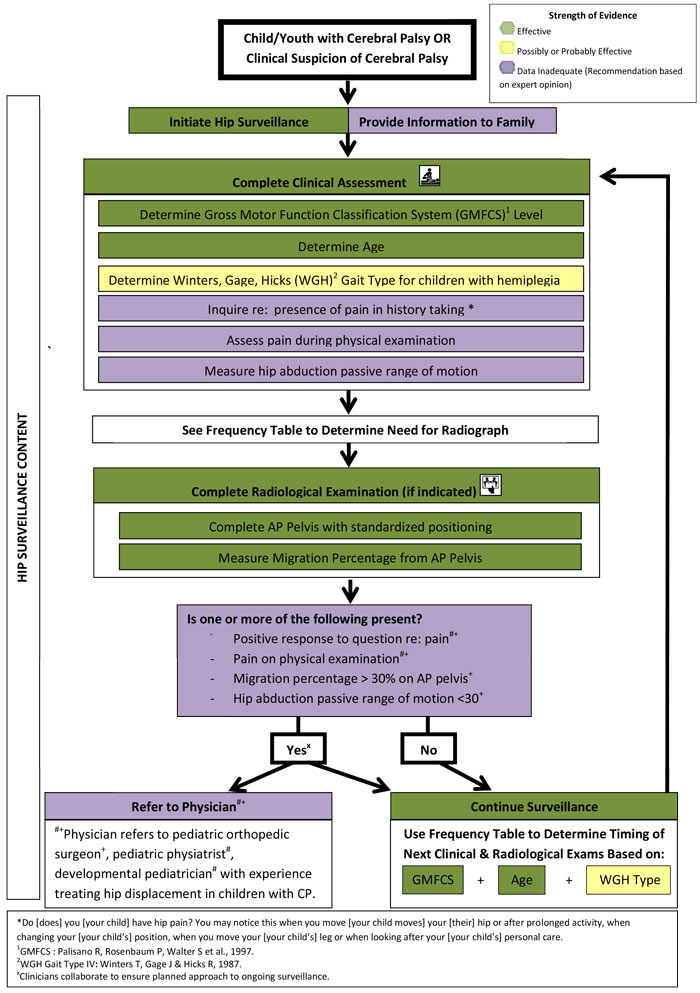
Hip surveillance involves a multi-step process for every child with CP.
Surveillance consists of two components: aclinical examination and a radiographic examinationwhich are completed at surveillance intervals which vary according to risk. The clinical examination involves determining/re-confirming, age, Gross Motor Function Classification System (GMFCS) level and Winters, Gage, Hicks (WGH) gait type at each surveillance interval in addition to inquiring re: pain during history taking. Hip abduction passive range of motion (PROM) is also measured with attention given to presence of pain on assessment.
Radiographic examination consists of measurement of migration percentage (MP) from a supine AP pelvis radiograph with standardised positioning.
Frequency
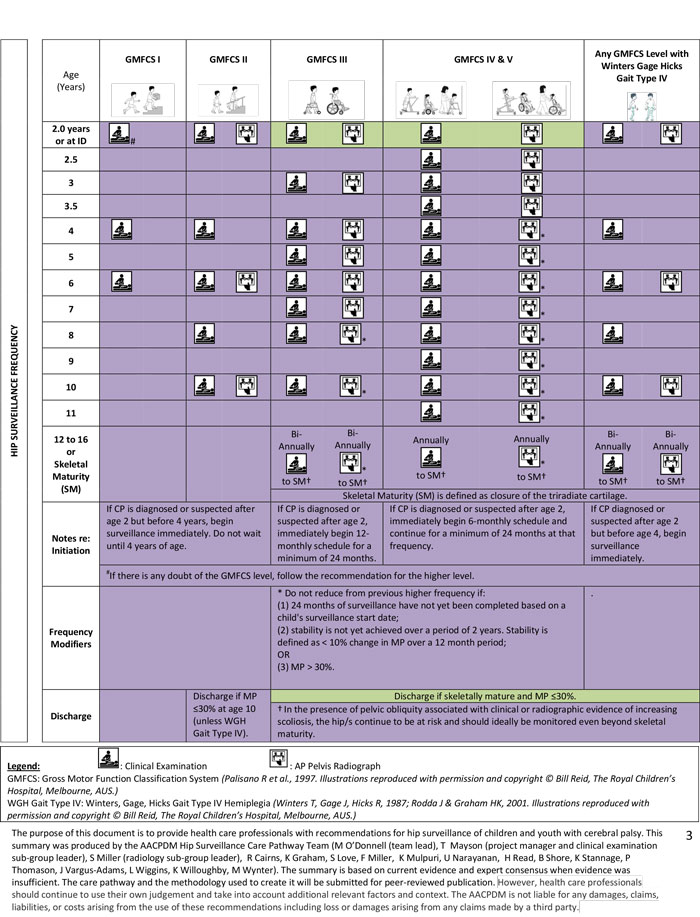
Surveillance frequency is based on a child’s age, GMFCS level, and WGH gait type. Surveillance is ideally initiated by 2 years of age, when a CP diagnosis is provided, or when CP is suspected. Surveillance frequency increases with increasing GMFCS level; frequency modifiers are based on absolute MP value and percentage change in MP.
Discharge criteria vary depending on GMFCS level and WGH gait type. Children at GMFCS levels III to V and those with a WGH Gait Type IV hemiplegia are discharged at skeletal maturity except those with a MP greater than 30% or those with pelvic obliquity in the presence of increasing scoliosis where continued surveillance is recommended. Children at GMFCS levels I and II are discharged earlier if MP is stable and under 30%.
Referral
Referral to a pediatric physiatrist, developmental paediatrician orpediatricorthopedic surgeon with experience treating hip displacement in children with CP is recommended when there is presence of hip pain on history and/or physical examination. When the migration percentage is greater than 30% and/or there is less than 30 degrees of hip abduction with or without other findings, referral to a pediatric orthopaedic surgeon is recommended.
Section II: Published Evidence
The published l iterature was reviewed to determine the effectiveness of hip surveillance in children with cerebral palsy as well as the elements that should be i ncluded in hip surveillance and their recommended frequency. The Hip Surveillance Care Pathway is based on this current best evidence as well as expert consensus when evidence was not available. The care pathway and the methodology used to create it will b e submitted for peer - reviewed publication.
Evidence for Hip Surveillance Effectiveness:
The literature supports the completion of hip surveillance in children and youth with cerebral palsy.
Gordon GS & Simkiss DE . A systematic review of the evidence for hip surveillance in children with cerebral palsy. J Bone Joint Surg - Br 2006; 88 - B : 1492 - 6. doi:10.1302/0301 - 620X.88B. 18114.
Hagglund G, Alriksson - Schmidt A, Lauge - Pedersen H, Rodby - Bousquet E, Wagner P, Westbom L. Prevention of dislocation of th e hip in children with cerebral palsy: 20 - year results of a population - based prevention programme. Bone Joint J 2014; 96 - B : 1546 - 52. doi: 10.1302/0301 - 620X.96B.34385.
Wynter M, Gibson N, Willoughby KL, et al. Australian hip surveillance guidelines for children with cerebral palsy: 5 - year review. Dev Med Child Neurol 2015; 57 : 808 - 20. doi: 10.1111/dmcn.12754.
Evidence for Hip Surveillance Clinical Exam ination and Hip Health Practical Tool Content:
The literature supports that hip surve illance be based on a chil d’s age and G ross M otor F unction C lassification S ystem . The additional content of the clinical exam ination component of the Hip Surveillance Care P athway as well as the Hip Health Practical Tool was established through expert consensus after review of the literature.
Wynter M, Gibson N, Willoughby KL, et al. Australian hip surveillance guidelines for children with cerebral palsy: 5 - year review. Dev Med Child Neurol 2015; 57 : 808 - 20. doi: 10.1111/dmcn.12754.
Evidence for Hip Surveillance Radiographic Exam ination and Radiography Practical Tool Content:
The literature supports hip surveillance based on a child’s migration percentage as measured on an AP pelvis radiograph taken with standardized positioning. The content of the Hip Surveillance Care P athway an d the Radiography Practical Too l was established through expert consensus after review of the literature. A review of this literature will be submitted for peer - reviewed publication.
Hagglund G, Lauge - Pedersen H, Persson M. Radiographic threshold value s for hip screening in cerebral palsy. J Child Orthop 2007; 1 : 43 – 7.
Parrott J, Boyd RN, Dobson F, et al. Hip displacement in spastic cerebral palsy: repeatability of radiologic measurement. J Pediatr Orthop 2002; 22 : 660 – 7.
Pons C, Remy - Neris O, Medee B , Brochard S. Validity and reliability of radiological methods to assess proximal hip geometry in children with cerebral palsy: a systematic review. Dev Med Child Neurol 2013; 5 : 1089 - 102. doi: 10.1111/dmcn.12169 . 5
Evidence for Hip Surveillance Frequency
The content of the care pathway was established through expert consensus after review of the literature and comparison of currently existing international hip surveillance programs in Australia (Consensus Statement on Standards of Care) , Canada ( Britis h Columbia Provincial Hip Surveillance Program; Holland Bloorview Kids Rehabilitation Hospital, Ontario; Grandview Children’s Centre , Ontario ) ; USA (Boston Children’s Hospital, Boston, MA; Alfred I. DuPont Hospital for Children, Wilmington, DW) ; Swede n (CP UP) ; United Kingdom (Bristol, Scotland). Program comparisons will be submitted for peer - reviewed publication.
Wynter M, Gibson N, Willoughby KL, et al. Australian hip surveillance guidelines for children with cerebral palsy: 5 - year review. Dev Med Child Neurol 2015; 57 : 808 - 20. doi: 10.1111/dmcn.12754.
Section III: Practical Tools
Gross Motor Function Classification System (GMFCS)
For information regarding the GMFCS, please see:
Palisano R, Rosenbaum P, Walter S, Russell D, Wood E, Galuppi B. Development and reliability of a system to clas sify gross motor function in children with cerebral palsy. Dev Med Child Neurol 1997; 3 : 214 - 23.
Winters, Gage, Hicks (WGH) Type IV Gait Pattern in Children with Hemiplegia
For information regarding the WGH Type IV gait in children with hemiplegia, please see: Winters T, Gage J, H icks R. Gait patterns in spastic hemiplegia in children and young adults. J Bone Joint Surg Am. 1987; 69 : 437 - 441.
Rodda J & Graham HK . Classification of gait patterns in spastic hemiplegia and spastic diplegia: a basis for a management algorithm. Eur J Neurol. 2001; 8 (S5):S98 - 108
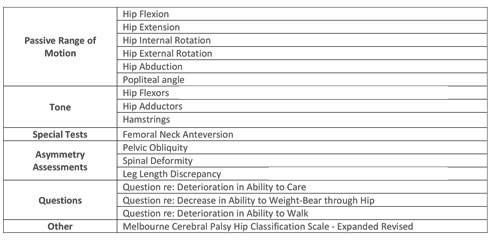
Hip Health Addendum Practical Tool
Hip surveillance is one component in the musculoskeletal care of children with cerebral palsy. As part of the ‘Hip Surveillance Pathway’ consensus building process, various measures, tests and clini cal questions were identified by the expert panel as being helpful in supporting hip/musculoskeletal health.
While these items were not identified as being necessary for hip surveillance, the consensus panel agrees that the following list of measures are worthy of your consideration as you evaluate hip health on an ongoing basis for children with cerebral palsy.
Radiography Addendum Practical Tools
1. Anterio - posterior (AP) Pelvis Radiograph Positioning
A supine AP pe lvis radiograph in a standardized position is required to accurately measure migration percentage (MP). MP values can be impacted by hip abduction (MP may measure low) and adduction (MP may measure high) so femurs should be positioned in neutral adduction /abduction. Measurement of MP requires that the triradiate cartilages be visible and therefore anterior and posterior pelvic tilt must be corrected. Position with neutral pelvic obliquity and flattened lordosis. Position as close to optimal as possible.
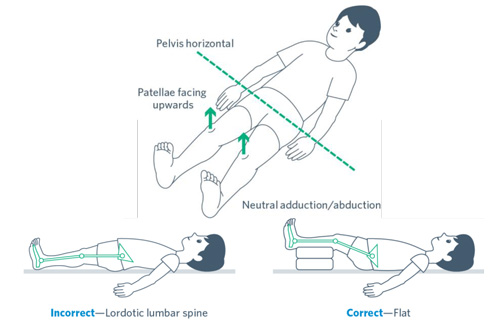
Reproduced with permission and copyright © Bill Reid, The Royal Children’s Hospital, Melbourne, Australia.
2. Field of View & Gonad Protection
An AP pelvis radiograph is recommended for hip surveillance. The ideal field of view will include the proxim al femurs; this allows for the assessment of whether the femurs were positioned in neutral abduction/adduction, as required for measuring migration percentage. Visualization of the iliac crests is recommended as it may be helpful in determining pelvic obl iquity and in assessing skeletal maturity using the Risser sign. Local gonad protection guidelines should be adopted. An example of the preferred fi eld of view is provided.

3. Measuring Migration Percentage
Reimer’s migration percentage (MP) is the recomme nded measurement to assess hip displacement. MP represents the portion of the ossified femoral head that is not covered by the ossified acetabular roof.
- 1. Draw Hilgenreiner's line (H) , a horizontal line between the superior aspect of the triradiate cartil ages. When the triradiate cartilages are closed, after skeletal maturity, the most useful horizontal line is through the most inferior points of the acetabular teardrops.
- 2. Draw Perkin’s line (P), perpendicular to Hilgenreiner’s line, at the lateral edge of the acetabulum ( see notes on identification of Gothic arch ).
- 3. Draw lines, parallel to Perkin’s line, along the medial and lateral side of the ossified femoral head.
- 4. Measure distance between medial and lateral sides of the femoral head (B).
- 5. Measure distanc e between Perkin’s line and lateral side of the femoral head (A). 6. Calculate MP (A/B x 100%).
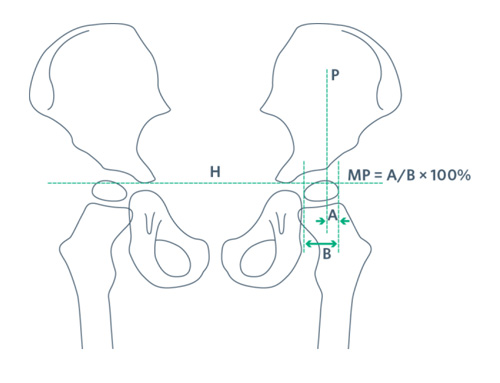
Reproduced with permission from Wynter M et al. Australian Hip Surveillance Guidelines for Children with CP; 2014.
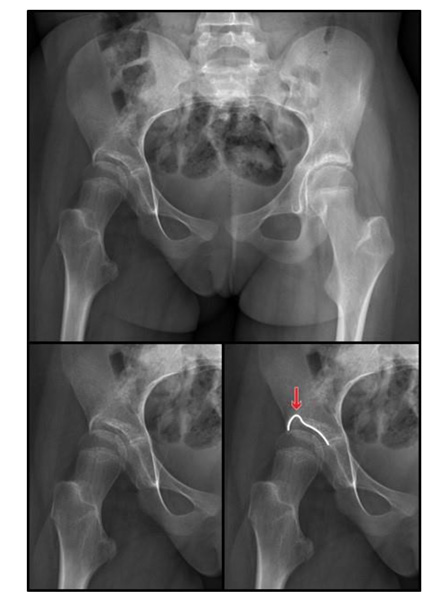
4. Identification of Gothic Arch
A “Gothic arch” results when eccentric pressure from a displaced femoral head causes the inhibition of ossification of the superolateral aspect of the cartilaginous acetabulum (Parrot t et al., 2002). When present, there is a risk that the measurement of MP could be underestimated. If a gothic arch is observed on x-ray, significant acetabular dysplasia is present, hip migration is likely significant, and it is recommended the child be referred to a pediatric orthopaedic surgeon. I t is recommended that the midpoint of the arch be used when placing Perkin’s line (Parrot t et al . , 2002; Hagglund et al . , 2007).
Section IV: Acknowledgments
| Name | Affiliation(s) | Location | Specialty Expertise |
|---|---|---|---|
| Maureen O’Donnell(Lead) | Child Health BC The University of British Columbia | Vancouver, BC, Canada | Developmental Pediatrician |
| Tanja Mayson (Project manager and subgroup lead) | Sunny Hill Health Centre for Children The University of British Columbia | Vancouver, BC, Canada | Physiotherapist Project Manager |
| Stacey Miller (Subgroup lead) | British Columbia Children’s Hospital The University of British Columbia | Vancouver, BC, Canada | Physiotherapist |
| Robyn Cairns | British Columbia Children’s Hospital The University of British Columbia | Vancouver, BC, Canada | Pediatric Radiologist |
| Kerr Graham | The Royal Children’s Hospital | Melbourne, VIC, Australia | Pediatric Orthopedic Surgeon |
| Sarah Love | Princess Margaret Hospital for Children | Perth, WA, Australia | Physiotherapist |
| Freeman Miller | Alfred I. DuPont Hospital for Children | Wilmington, DE, USA | Pediatric Orthopedic Surgeon |
| Kishore Mulpuri | British Columbia Children’s Hospital The University of British Columbia | Vancouver, BC, Canada | Pediatric Orthopedic Surgeon |
| Unni Narayanan | The Hospital For Sick Children & Holland Bloorview Kids Rehabilitation Hospital. University of Toronto | Toronto, ON, Canada | Pediatric Orthopedic Surgeon |
| Heather Read | Greater Glasgow and Clyde Health Board | Glasgow, Scotland | Pediatric Orthopedic Surgeon |
| Benjamin Shore | Boston Children’s Hospital | Boston, MA, USA | Pediatric Orthopedic Surgeon |
| Kate Stannage | Princess Margaret Hospital for Children | Perth, WA, Australia | Pediatric Orthopedic Surgeon |
| Pam Thomason | The Royal Children’s Hospital | Melbourne, VIC, Australia | Physiotherapist |
| Jilda Vargus-Adams | Cincinnati Children’s Hospital Medical Center | Cincinnati, OH, USA | Pediatric Physiatrist |
| Laura Wiggins | Greater Glasgow and Clyde Health Board | Glasgow, Scotland | Physiotherapist |
| Kate Willoughby | The Royal Children’s Hospital | Melbourne, VIC, Australia | Physiotherapist |
| Meredith Wynter | Queensland Paediatric Rehabilitation Service | Brisbane, QLD, Australia | Physiotherapist |

Feedback/Comments
The American Academy for Cerebral Palsy and Developmental Medicine has developed care pathways to assist the busy clinician. Please submit any advice or constructive feedback to make this pathway more useful.
NOTE: Feedback will be directed to the AACPDM Care Pathway Taskforce to review and consider on a queue 6-month basis.